Click here to Visit Facebook Page
Introduction:
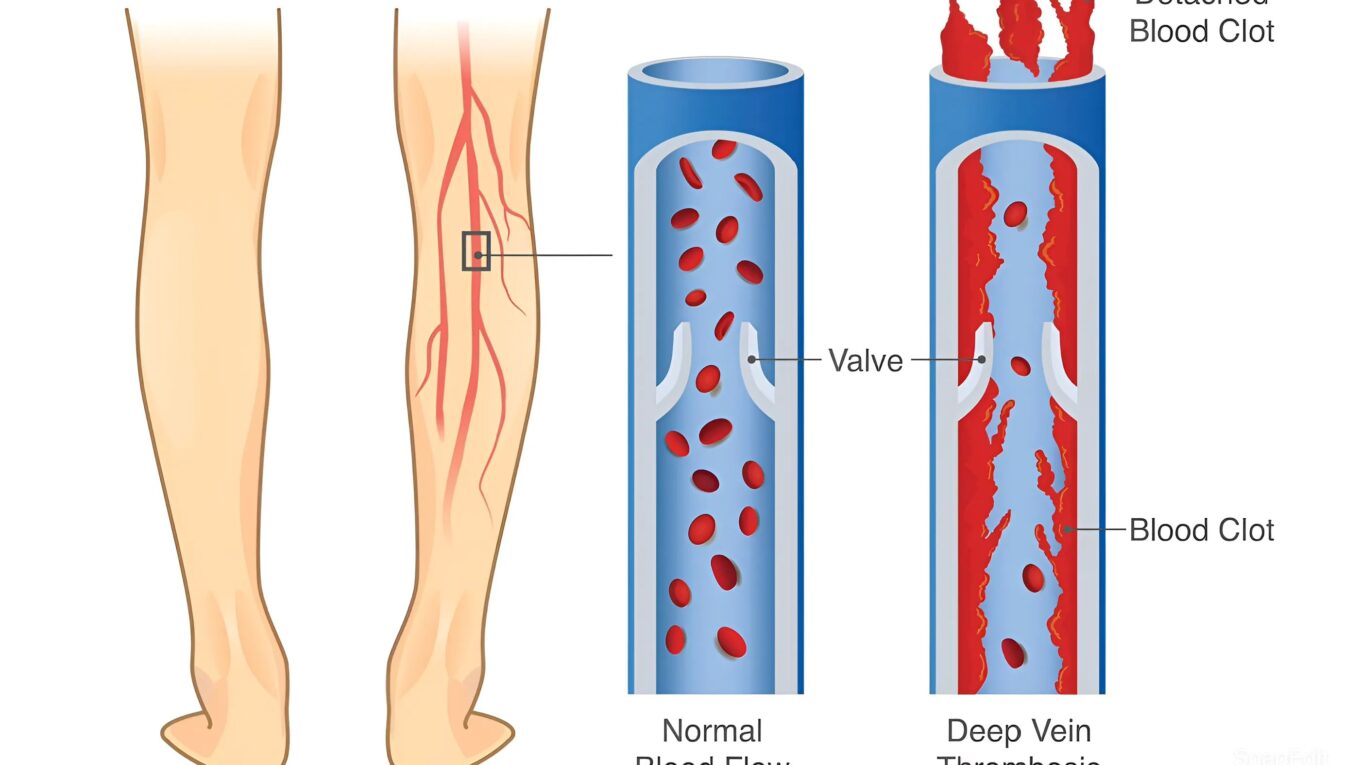
Understanding Deep Vein Thrombosis. Deep Vein Thrombosis (DVT) is a serious condition where a blood clot forms in a deep vein, typically in the legs. This condition can cause pain and swelling and, if left untreated, can lead to potentially life-threatening complications. This blog aims to provide an in-depth understanding of DVT, including its causes, symptoms, risk factors, diagnosis, treatment, and prevention.
What is Deep Vein Thrombosis?
Deep Vein Thrombosis occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body. This clot can partially or completely block the flow of blood through the vein. While DVT most commonly affects the legs, it can also occur in other parts of the body.
Click here to Visit Facebook Page
Causes of Deep Vein Thrombosis:
Several factors can contribute to the development of DVT, often categorized into three main groups known as Virchow’s triad:
1. Stasis of Blood Flow:
When blood flow is slow or stagnant, it increases the likelihood of clot formation. This can occur due to prolonged immobility, such as sitting for long periods during travel or bed rest after surgery.
2. Endothelial Injury:
Damage to the blood vessel lining can trigger clot formation. This damage can result from surgery, trauma, or inflammation.
3. Hypercoagulability:
Certain conditions and medications can make the blood more prone to clotting. These include genetic disorders, cancer, hormone replacement therapy, and birth control pills.
Click here to Visit Facebook Page
Symptoms of Deep Vein Thrombosis:
The symptoms of DVT can vary, and some individuals may experience no symptoms at all. Common symptoms include:
– Swelling in the affected leg or arm
– Pain or tenderness, often starting in the calf
– A feeling of warmth in the affected area
– Red or discolored skin
It is important to note that if a clot dislodges and travels to the lungs, it can cause a pulmonary embolism (PE), a severe condition characterized by:
– Sudden shortness of breath
– Chest pain or discomfort, which may worsen with deep breathing or coughing
– Rapid pulse
– Coughing up blood
Click here to Visit Facebook Page
Risk Factors for Deep Vein Thrombosis:
Several factors increase the risk of developing DVT, including:
– Prolonged Immobility:
Extended periods of inactivity, such as long flights or bed rest, can slow blood flow.
– Injury or Surgery:
Trauma or surgery involving the veins can increase the risk of clot formation.
– Certain Medications:
Hormone therapy, birth control pills, and some cancer treatments can elevate the risk.
– Chronic Medical Conditions:
Conditions like heart disease, cancer, and inflammatory bowel disease are linked to higher DVT risk.
– Genetic Factors:
A family history of DVT or inherited clotting disorders can increase susceptibility.
– Lifestyle Factors:
Smoking, obesity, and a sedentary lifestyle contribute to the risk of DVT.
Click here to Visit Facebook Page
Diagnosing Deep Vein Thrombosis:
If DVT is suspected, a healthcare provider will conduct a thorough evaluation, which may include:
– Physical Examination:
Checking for swelling, tenderness, and discoloration in the affected area.
– D-dimer Test:
A blood test that measures a substance released when a blood clot breaks up. High levels can indicate the presence of an abnormal blood clot.
– Ultrasound:
The most common method for diagnosing DVT, using sound waves to visualize blood flow and detect clots.
– Venography:
An X-ray test that involves injecting a contrast dye into a large vein in your foot or ankle to show the deep veins in your leg and any blood clots.
Click here to Visit Facebook Page
Treatment of Deep Vein Thrombosis:
Treatment aims to prevent the clot from growing, reduce the risk of pulmonary embolism, and avoid long-term complications. Common treatments include:
– Anticoagulants (Blood Thinners):
Medications like heparin, warfarin, and newer oral anticoagulants (NOACs) help prevent further clotting and reduce the risk of a PE.
– Thrombolytics:
In severe cases, these medications dissolve existing clots but come with a higher risk of bleeding.
– Compression Stockings:
These stockings help prevent swelling and reduce the risk of post-thrombotic syndrome, a condition characterized by long-term pain and swelling.
– Inferior Vena Cava (IVC) Filter:
For patients who cannot take anticoagulants, a filter can be inserted into the large vein in the abdomen to prevent clots from traveling to the lungs.
Click here to Visit Facebook Page
Preventing Deep Vein Thrombosis:
Prevention strategies focus on minimizing risk factors and improving blood circulation:
– Stay Active:
Regular exercise and avoiding prolonged periods of immobility are crucial.
– Hydration:
Drinking plenty of fluids helps maintain blood flow.
– Healthy Lifestyle:
Maintaining a healthy weight, avoiding smoking, and managing underlying medical conditions can reduce risk.
– Compression Stockings:
Wearing compression stockings during long trips or post-surgery can help improve blood flow.
– Medications:
For high-risk individuals, doctors may prescribe low-dose anticoagulants during periods of increased risk, such as post-surgery or long flights.
Click here to Visit Facebook Page
Conclusion:
Deep Vein Thrombosis is a serious medical condition that requires prompt attention and treatment. Understanding the causes, recognizing the symptoms, and being aware of the risk factors can help in early detection and prevention. If you suspect you have DVT or are at risk, consult a healthcare provider for proper evaluation and management. With appropriate care and lifestyle modifications, the risks associated with DVT can be significantly reduced, ensuring better overall health and well-being.