Click here to Visit Facebook Page
Introduction:
Tuberculosis (TB) is a severe infectious disease caused by the bacterium Mycobacterium tuberculosis. While TB primarily affects the lungs, it can also spread to other parts of the body, including the brain. When TB affects the membranes surrounding the brain and spinal cord, it results in a condition known as Tuberculosis Meningitis (TBM). This blog provides an in-depth look at TBM, covering its symptoms, diagnosis, treatment, and prevention strategies.
Click here to Visit Facebook Page
What is Tuberculosis Meningitis?
Tuberculosis Meningitis is a life-threatening condition where the tuberculosis bacteria infect the meninges, the protective membranes covering the brain and spinal cord. It is one of the most severe forms of extrapulmonary tuberculosis, requiring prompt diagnosis and treatment to prevent serious complications or death.
Click here to Visit Facebook Page
Causes and Pathogenesis:
TBM occurs when Mycobacterium tuberculosis spreads from an initial infection site, typically the lungs, to the central nervous system (CNS). This spread usually happens through the bloodstream. Once in the CNS, the bacteria cause inflammation of the meninges, leading to the symptoms associated with TBM.
Click here to Visit Facebook Page
Symptoms:
The symptoms of TBM can develop gradually over several weeks and may initially be nonspecific, making early diagnosis challenging. Key symptoms include:
1. Persistent Headache: Often severe and not relieved by standard painkillers.
2. Fever: Low-grade but persistent.
3. Neck Stiffness: Difficulty in bending the neck forward.
4. Nausea and Vomiting: Often due to increased intracranial pressure.
5. Altered Mental Status: Confusion, lethargy, or even coma in severe cases.
6. Photophobia: Sensitivity to light.
7. Seizures: Occur in some cases due to the inflammation of brain tissue.
8. Cranial Nerve Palsies: Weakness or paralysis of muscles controlled by cranial nerves.
Click here to Visit Facebook Page
Diagnosis:
Early diagnosis of TBM is critical but challenging due to the nonspecific nature of early symptoms. Several diagnostic tools and procedures are employed:
1. Clinical Evaluation:
A thorough history and physical examination focusing on TB exposure and neurological symptoms.
2. Lumbar Puncture (Spinal Tap):
Analysis of cerebrospinal fluid (CSF) for elevated protein, low glucose levels, and the presence of Mycobacterium tuberculosis.
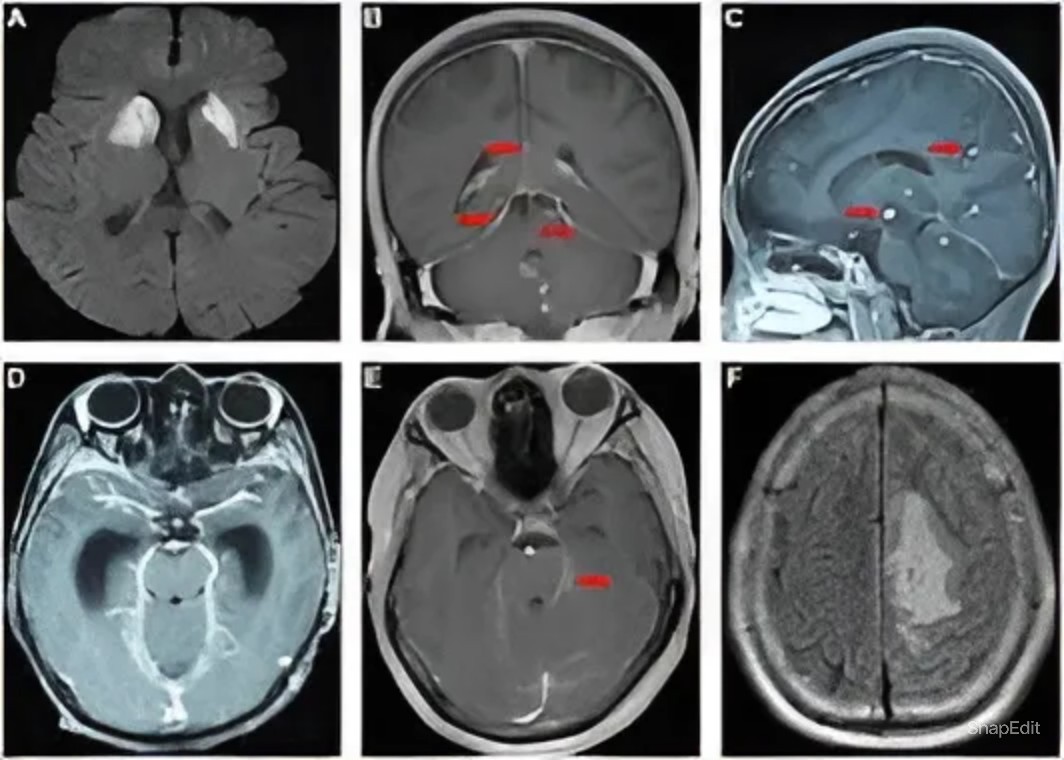
3. Imaging:
MRI or CT scans of the brain can show meningeal enhancement, hydrocephalus, or tuberculomas.
4. Microbiological Tests:
CSF culture, Ziehl-Neelsen stain, and nucleic acid amplification tests (NAAT) like PCR to detect TB bacteria.
5. Tuberculin Skin Test (TST) or Interferon-Gamma Release Assays (IGRAs):
These tests can support the diagnosis but are not definitive for TBM.
Click here to Visit Facebook Page
Treatment:
Treatment of TBM is prolonged and requires a combination of antibiotics and supportive therapies:
1. Antituberculosis Drugs:
A regimen including isoniazid, rifampin, pyrazinamide, and ethambutol for the initial 2 months, followed by isoniazid and rifampin for at least 10 months. This extended treatment period is necessary due to the bacteria’s ability to persist in the CNS.
2. Adjunctive Corticosteroids:
Prednisone or dexamethasone to reduce inflammation and prevent complications such as brain edema and infarctions.
3. Management of Complications:
Treatment of hydrocephalus with surgical shunting if necessary, and addressing other complications like seizures.
Click here to Visit Facebook Page
Prognosis:
The prognosis of TBM largely depends on the stage at which treatment is initiated. Early diagnosis and prompt treatment significantly improve outcomes. However, delayed treatment can result in severe neurological deficits or death. Long-term complications can include cognitive impairments, motor deficits, and other neurological dysfunctions.
Click here to Visit Facebook Page
Prevention:
Preventing TBM involves controlling the spread of TB through several strategies:
1. BCG Vaccination:
Bacillus Calmette-Guérin (BCG) vaccine is given to children in TB-endemic areas to provide some protection against TB, including TBM.
2. Early Detection and Treatment of Pulmonary TB:
Reducing the reservoir of infection and preventing the spread to other parts of the body.
3. Infection Control Measures:
Use of protective masks, good ventilation, and isolation of infectious patients in healthcare settings.
4. Prophylactic Treatment:
In individuals with latent TB infection or those who have been in close contact with TB patients.
Click here to Visit Facebook Page
Conclusion:
Tuberculosis Meningitis is a severe and potentially fatal condition requiring immediate medical attention. Awareness of its symptoms, early diagnosis, and appropriate treatment are crucial in improving patient outcomes. Public health measures, including vaccination and effective TB control programs, play a significant role in preventing TBM. By understanding and addressing this condition, we can reduce its impact and save lives.